What is Graves' Disease?
Graves’ disease is the most common cause of hyperthyroidism, a condition in which the thyroid gland becomes overactive and produces more thyroid hormones than the body needs. Because thyroid hormones help regulate metabolism, energy production, heart rate, digestion, and temperature, Graves’ disease can affect nearly every organ system. While the condition can occur in any gender or age group, it’s significantly more common in women and often appears in early to mid-adulthood.
Graves’ disease is autoimmune, as in, the immune system mistakenly attacks healthy cells. In this case, the immune system produces antibodies that overstimulate the thyroid gland, causing it to produce excess hormones.
Understanding the Thyroid
The thyroid is a small, butterfly-shaped gland at the base of the neck. Its hormones (T3 and T4) are responsible for maintaining metabolic balance, supporting the nervous system, influencing heart rhythm, and helping regulate digestion and energy.
In Graves’ disease, the immune system produces an antibody called thyroid-stimulating immunoglobulin (TSI). TSI attaches to the same receptors the brain uses to regulate thyroid hormone production, but instead of maintaining balance, it continually signals the thyroid to produce more hormones. As levels of circulating thyroid hormone rise, the body begins operating in a “high-speed” state, which leads to the wide range of symptoms associated with hyperthyroidism.
While a visible swelling of the thyroid (goiter) sometimes occurs, many people don’t have outward physical changes, especially early in the disease. Symptoms can be subtle at first, which is why Graves’ disease is sometimes overlooked until thyroid hormone levels become significantly elevated.
What Causes Graves’ Disease?
Researchers agree that Graves’ disease is caused by a combination of genetic susceptibility and environmental triggers. In other words, some individuals inherit a tendency toward autoimmune thyroid conditions, but the condition typically develops only after certain external or internal factors influence the immune system.
Genetics
People with a family history of Graves’ disease or other autoimmune disorders have a higher likelihood of developing the condition themselves.
Immune system dysregulation
Autoimmune thyroid diseases develop when immune tolerance breaks down, allowing the body to attack its own tissues. Once the immune system begins producing TSI antibodies, the thyroid becomes overstimulated.
Major triggers
Certain life events or exposures may contribute to the onset of Graves’ disease in individuals who are already genetically susceptible. These may include:
Significant emotional or physical stress, which has measurable effects on the immune system.
Pregnancy and postpartum immune shifts, which temporarily alter immune balance.
Smoking, which is strongly associated with the development and worsening of Graves’ eye disease.
Viral or infectious exposures, which may stimulate abnormal immune responses.
Nutrient deficiencies, such as low selenium, low vitamin D, or inadequate intake of key minerals involved in thyroid regulation.
Iodine excess, which can overstimulate the thyroid in susceptible individuals.
Gut health disturbances, including increased intestinal permeability and microbial imbalance, which may contribute to overall immune dysfunction.
Environmental exposures, such as endocrine-disrupting chemicals or pollutants.
Not every person with these risk factors develops Graves’ disease, but these influences may help explain why the immune system becomes overactive in some individuals and not in others.
Common Symptoms of Graves’ Disease
Thyroid hormones play a central role in metabolism, so symptoms of Graves’ disease reflect the body’s response to elevated hormone levels. The severity of symptoms varies widely: some people experience pronounced symptoms, while others have more subtle changes that progress over time.
General symptoms
Unintentional weight loss
Increased appetite
Rapid or irregular heartbeat
Anxiety, restlessness, or irritability
Heat intolerance or excessive sweating
Shakiness or tremors
Muscle weakness, especially in the upper arms and thighs
Difficulty sleeping
Fatigue despite feeling “wired”
More frequent bowel movements
Enlarged thyroid (goiter)
Eye changes
Some individuals develop Graves’ ophthalmopathy, an autoimmune condition affecting the tissues surrounding the eyes. Symptoms may include:
Redness, dryness, or irritation
A feeling of pressure behind the eyes
Bulging or protrusion of the eyes
Light sensitivity
Double vision
This condition varies significantly in severity and does not always correlate with the level of thyroid hormone elevation.
Skin changes
A small number of people develop thickened skin over the shins, called pretibial myxedema.
Symptoms in women
Because thyroid hormones interact with reproductive hormones, women may experience:
Irregular or lighter menstrual cycles
Difficulty conceiving
Increased risk of complications during pregnancy if hyperthyroidism is untreated
Thyroid storm
Thyroid storm is a rare but life-threatening medical emergency. It involves a sudden and extreme rise in thyroid hormone activity, causing severe fever, a dangerously high heart rate, confusion, and organ dysfunction. Prompt treatment is essential.
Who is at Risk for Graves’ Disease?
While Graves’ disease can affect anyone, the likelihood is higher in:
Women
Individuals with a family history of autoimmune disease
People with other autoimmune conditions
Smokers
Those who have recently experienced significant stress or hormonal shifts
Individuals with high iodine exposure from supplements or medical procedures
How is Graves’ Disease Diagnosed?
Diagnosis typically involves a combination of symptom evaluation, physical examination, and laboratory testing.
Blood tests
Bloodwork is essential in confirming Graves’ disease. The following markers are commonly evaluated:
TSH (thyroid-stimulating hormone): Usually very low or suppressed.
Free T3 and Free T4: Typically elevated.
TSI (thyroid-stimulating immunoglobulin) and TRAb (TSH receptor antibodies): Help confirm the autoimmune nature of the condition.
TPO antibodies: May be elevated in autoimmune thyroid disease but are not specific to Graves’.
Imaging
Additional tests may include:
Thyroid ultrasound, which can detect increased blood flow through the gland and identify structural changes.
Radioactive iodine uptake (RAIU), which measures how actively the thyroid absorbs iodine; high uptake is characteristic of Graves’ disease.
Doppler flow studies, which can also assess thyroid blood flow.
These diagnostic tools help distinguish Graves’ disease from other causes of hyperthyroidism, such as thyroiditis or toxic nodular goiter.
Conventional Treatment Options
Treatment for Graves’ disease focuses on lowering thyroid hormone levels, relieving symptoms, and preventing long-term complications. The most appropriate therapy depends on age, pregnancy status, symptom severity, and personal medical history.
Anti-thyroid medications
Medications such as methimazole or propylthiouracil (PTU) reduce thyroid hormone production by blocking the enzymes involved in thyroid hormone synthesis. Methimazole is the most commonly used medication, while PTU is preferred during the first trimester of pregnancy or when methimazole is not tolerated.
Beta blockers
These medications don’t treat the underlying autoimmune condition but are often used to quickly relieve symptoms such as rapid heartbeat, tremors, and anxiety.
Radioactive iodine therapy
This therapy uses a small dose of radioactive iodine to selectively destroy overactive thyroid cells. Over time, this reduces thyroid hormone output. Many people treated with radioactive iodine eventually develop hypothyroidism and require lifelong thyroid hormone replacement.
Thyroid surgery
Surgical removal of part or all of the thyroid gland may be recommended when other treatments are not suitable, such as in cases of very large goiters, severe eye disease, or pregnancy when medications are not effective or tolerated.
Supporting Long-Term Health With Graves’ Disease
Managing Graves’ disease extends beyond lowering thyroid hormone levels. Because the condition is autoimmune in nature, supporting overall immune balance and general health can be extremely helpful.
Nutrient support
Adequate levels of certain nutrients contribute to healthy thyroid function and immune balance. These may include:
Selenium, which supports normal thyroid hormone metabolism
Vitamin D, which plays a role in immune regulation
Zinc and iron, which contribute to thyroid hormone production and overall metabolic health
Testing may be helpful to determine whether supplementation is appropriate.
Gut health
Restoring digestive balance and supporting the intestinal barrier may help reduce immune activation in some individuals, especially if there are coexisting gut symptoms or known sensitivities.
Stress management
Because stress influences hormone regulation and immune activity, incorporating practices such as meditation, deep breathing, gentle movement, or counseling may reduce symptom flares and improve overall well-being.
Nutrition
Many people feel better with a nutrient-dense, anti-inflammatory eating pattern that includes vegetables, fruits, lean proteins, fiber, and healthy fats. Some individuals may benefit from limiting excess iodine from supplements or reducing foods that aggravate symptoms.
Avoiding smoking
Smoking is one of the strongest modifiable risk factors for worsening eye symptoms in Graves’ disease.
Living With Graves’ Disease
With appropriate treatment and regular monitoring, most people with Graves’ disease lead healthy, active lives. It is important to work closely with a healthcare provider to ensure that thyroid levels remain stable and that symptoms or complications are addressed early.
Managing Graves’ disease may involve:
Ongoing thyroid testing
Medication adjustments as needed
Attention to nutrition and lifestyle factors
Eye evaluations when appropriate
Special monitoring during pregnancy
Early diagnosis, consistent follow-up, and a comprehensive approach to health can significantly improve long-term outcomes.
Where Can I Learn More About Managing Graves’ Disease?
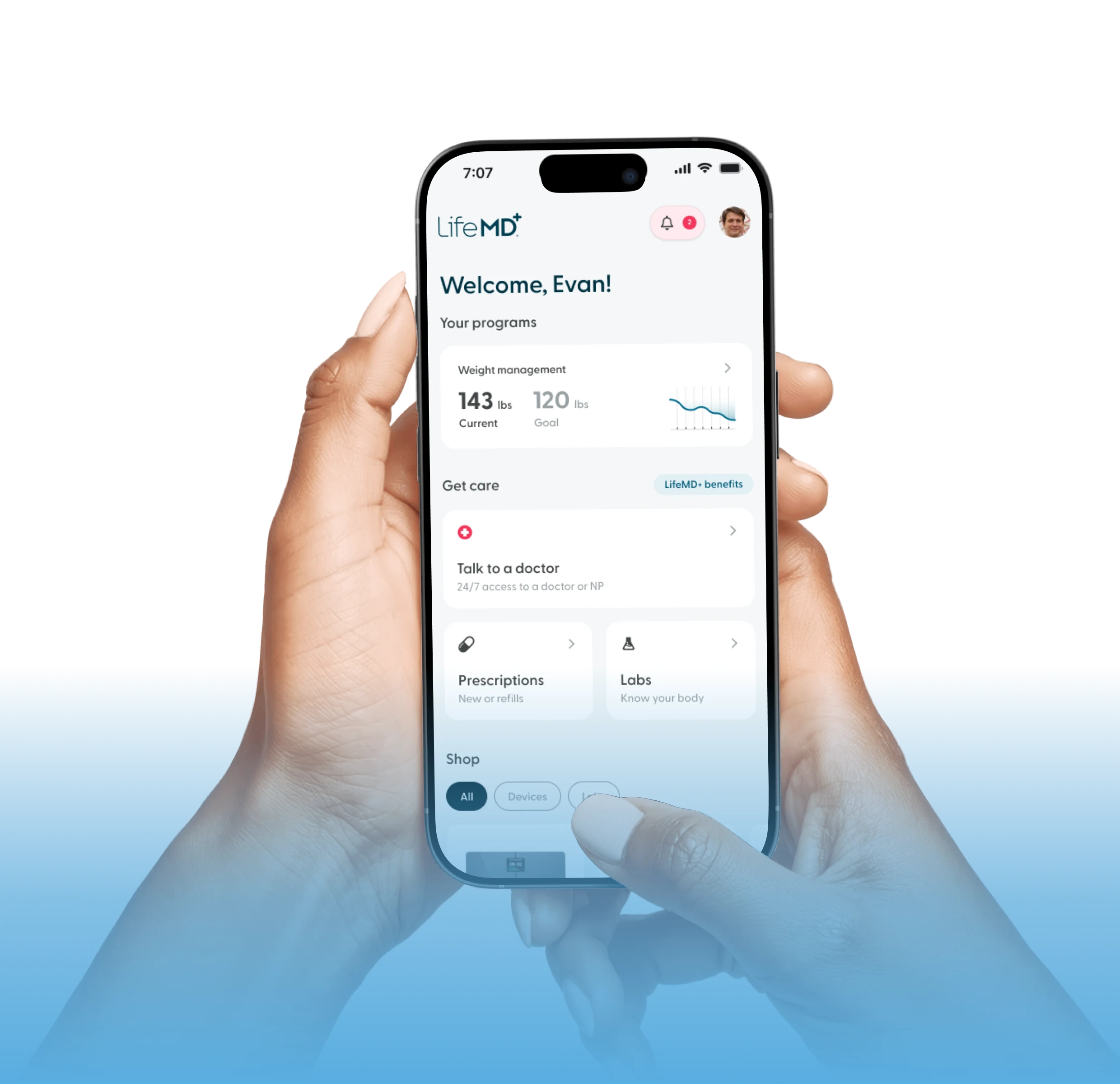
Symptoms of hyperthyroidism are often similar to menopausal symptoms. A LifeMD-affiliated healthcare provider can help you develop a treatment plan for managing Graves’ disease and other common women’s health conditions like menopause.
With a LifeMD membership, you can access educational resources about women’s health, advice from licensed healthcare professionals, and prescription Graves’ disease medications if you qualify.
LifeMD allows members to meet with a healthcare provider in under an hour to find treatment to relieve Graves’ disease symptoms and other women’s health conditions.
Get started today by finding out what treatment options may work for you.